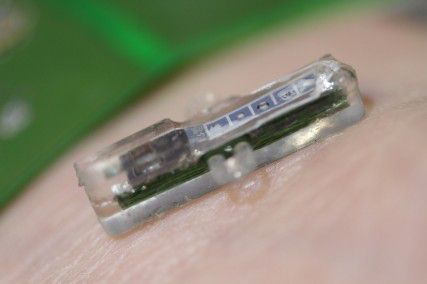
Researchers at École Polytechnique Fédérale de Lausanne, a research university in Switzerland, developed a small device that can be inserted a centimeter beneath the skin and monitor patients’ blood without a doctor’s visit.
The blood is the information highway of the body. By accessing its secrets, doctors can make more accurate diagnoses, assign better treatments and keep patients healthy. This can be seen in a variety of television shows, from the fiction series House to the documentary series, Medical Mysteries.
However, the importance of blood work is not unique to television shows. Patients undergoing treatment for cancer, organ transplants and other chronic illnesses have blood drawn on a regular basis — in some cases, this is every hour.
These types of patients were in the minds of researchers Sandro Carrara and Giovanni de Micheli of the École Polytechnique Fédérale de Lausanne, a research university in Switzerland.
In a March 20 EPFL press release, Carrara and De Micheli announced the development of a small device that can be inserted beneath the skin and monitor the blood of patients without a trip to the doctor.
A tiny laboratory
Carrara and De Micheli said they wanted to develop technology that would make the process of blood work easier for both patients and doctors.
Their new device — which is about a half an inch long — consists of five biosensors in a membrane that is inserted about a centimeter beneath the skin. These biosensors comb through the blood in search of molecules that trigger whatever doctors are searching for.
“By choosing which kind of probe molecules — which enzymes we plug on top of our sensors — we can decide to target different molecules,” Carrara said.
He said this means that doctors will be able to utilize this technology in diabetes patients, chemotherapy patients, and in other illnesses.
Once the device’s biosensors have collected the data, information is transferred through a small battery patch that is placed on the skin over the device, according to the press release. This patch powers the device with one-tenth a watt of power and communicates with it through radio frequency signals.
These signals are then sent to a doctor through a telephone or neighborhood collection device.
De Micheli said this patch is more ideal than inserting batteries under the skin.
“We don’t want to put batteries inside the human body and we don’t want to have wires because wires are typical vehicles of infection,” De Micheli said.
He said this patch also enables doctors to replace batteries without removing the device.
Carrara said some scientists expressed concerns with the design because devices in the blood often become clogged. However, he said this is not an issue.
“The clogging is solved by the fact that we use to protect our sensor a commercially viable membrane,” he said.
Carrara said the membrane is FDA approved and has been proven to stop the clogging of the biosensor.
Its significance
Researchers said the device will make blood testing simpler for patients, especially those living far away from hospitals and in rural areas. For these patients, getting blood work done every day — and sometimes every hour — is not viable.
With this development, however, patients would only need to leave their homes in the case of a medical emergency or to remove the device.
“The patient does not even have to remember about the test and it gets done,” De Micheli said. “The information is transmitted to the doctor or the medical provider.”
Michael Stephenson, a freshman in the School of Engineering, said he thinks this concept could be helpful for a variety of patients.
“I think for a lot of people — especially in a lot of different parts of the world where there is an undersupply of doctors, and people have to travel a long distance to see a doctor — having access to something like this, it would be a lot simpler for them,” Stephenson said.
Lissy Rosner, a freshman in the School of Education, said the device could help patients lead more normal lives.
“I think that this device would help people with chronic illness forget that they have that illness,” Rosner said. “For example, if they were in school they wouldn’t have to leave so often and it wouldn’t affect their lives as much.”
Researchers said this device will also aid in the regulation of drugs.
“In the case of chemotherapy or in the case of organ transplants it is very important to measure the exact dose of drug in the blood stream,” said De Micheli. “This is extremely important in order to have efficient personalized medicine.”
With this new access, doctors would be able to monitor their patients more closely and check their blood more frequently.
“We can also monitor pharmaceutical compounds that have been supplied to the patients in order to correlate the progress of the disease with the amount of the drug compound in the patients’ bodies,” Carrara said.
He said closer control of drug dosages will allow doctors to be more precise in treatments and could increase the success rates of chemotherapy and organ transplants.
Elbert Foo, an ENG freshman, said he was excited by this aspect of the device.
“I think this is a great advancement for the betterment of humanity and science,” Foo said. “It’s easy and convenient at the same time.”
Sargent College of Health and Rehabilitation Sciences freshman Jason Kim said he agreed with Foo.
“The technology is very accessible, so more people could get easy access to quick and easy medicine,” Kim said.
The challenges
Carrara and De Micheli said one of the biggest challenges in developing this technology was the cost. To squeeze technology of this caliber onto a silicon plate the size of a small safety pin has been extraordinarily expensive.
“On one side, we have nano-materials, we have soft materials, proteins, and of course we have metals on silicon,” Carrara said. “It has been a huge challenge in such a tiny space.”
To combat this, De Micheli said that he and other researchers tried to make the device as multifunctional as possible.
“We think we have achieved a platform that can be programmed chemically to sense different types of compounds, and as a result this can be used to treat and to monitor various pathologies with a lower cost because it’s versatile,” De Micheli said.
Researchers said another challenge involved the enzymes that the device uses, which have a relatively short life span.
“We are still limited by the duration and the degradation of some of the chemicals, the enzymes, that are used for doing the detection,” De Micheli said. “The implant, as it is now, can last for one to two months. We hope that we can have longer times.”
With further research and testing, Carrara and De Micheli said these devices will soon have longer life spans, which will increase effectiveness and decrease costs.
The scientific wait
Like many new developments in science, Carrara and De Micheli said the system needs more tweaks until it is ready for distribution. In the meantime, the product is being tested on mice.
“We have tested it for functionality. The test was positive, and of course we look forward to an entire path of tests on larger animals and eventually on humans,” De Micheli said.
Both scientists said the path to human testing is a long one on which they are just beginning. However, they said this technology will be licensed to test humans in about five years.
After four years of working to develop this technology, another five years seems daunting, but both researchers said they are determined to perfect this tiny device.
Part of the researchers’ enthusiasm stems from the response they received when they announced their invention.
“I think the biggest success is the interest in medical doctors, the interest of patients that call us that really would like to test it and use it,” De Micheli said. “We have to tell them that we have to go through the whole experimentation path before operating on them, but I think all this is very encouraging.”