Boston University researchers, as part of a study published in the Journal of the American Geriatric Society, have developed a method that will allow people to predict their five-year risk of requiring life support, according to a Wednesday press release from the Boston University Medical Center. The method uses existing medical records to calculate an individual’s risk of needing a mechanical ventilator within five years.
“The need for mechanical ventilation during critical illness represents an event of significant short- and long-term consequence. Patients requiring mechanical ventilation have approximately 30 percent hospital mortality rates, a substantial risk of near-term death,” the press release stated.
The study examined physical traits and genetic patterns in order to determine risk score. A risk score is a numerical representation of an individual’s risk for requiring life support and is affected by age, gender and medical history, according to the press release.
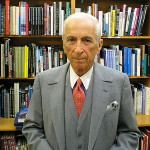
Allan Walkey, a professor of medicine at BU School of Medicine and one of the authors of the study, said the risk score would allow patients to maintain greater control over their own lives.
“It’s too late once you’re on life support to tell anyone what your wishes would be because you can’t communicate or talk,” Walkey said. “The goal is for people to express their wishes to their doctor beforehand. Unfortunately, that does not happen much, so people are left guessing as to what their loved ones or what their patients might want, and it’s important to get it right.”
He said he hopes risk score will give people more time to make difficult decisions and allow doctors to prioritize patients who have the highest risk of requiring life support.
Researchers of the study used data from the Framingham Heart Study, selecting data from participants over the age of 65 who had enrolled in Medicare. By combining the Framingham Heart Study data with Medicare data, researchers were able to create an extensive medical profile for each participant, Walkey said.
“I could link that data to their Medicare data to find out things about them that weren’t related to the Framingham Heart Study, and I was interested in seeing if we could predict which patients would go on to require a need for life support later in life,” he said.
According to the release, after analyzing Medicare records and data from the Framingham Heart Study, researchers identified certain factors that affect risk score. Factors that contribute to a higher risk of requiring life support include increasing old age, male sex, a history of heart failure or atrial fibrillation, a history of alcohol abuse and a hospitalization within the past year.
Researchers assigned points to each of these factors and then developed a scoring system for calculating risk score, the press release stated.
The factors that contribute to a risk of needing life support are easy for doctors and patients to identify, Walkey said.
“That’s what we thought was a strength of the score, is that people could just know and calculate it themselves or their doctor could calculate it for them, or even a computer could calculate it for them automatically by extracting things from their medical record,” Walkey said.
Although risk scores could provide patients and doctors with an accessible method of predicting future needs for life support, risk score is limited in that it is only based on research and statistics, Walkey said.
Walkey acknowledged that risk score is not absolute and says doctors would need to consult with their patients in order to determine what action should be taken.
“The risk score is a pretty objective thing,” he said. “It uses numbers and equations, and we need to compare that with more subjective measures and see whether doctors think someone is really sick without using that specific score.”
At the very least, Walkey said, he hopes the results of the study will increase communication between doctors and patients, ensuring that people are properly cared for.
“If it’s something that patients and doctors felt comfortable with and it increases the discussions between people, my hope is that, in the end, more people will be having these discussions with their doctors about what they want,” he said, “and that we are able to take better care of people towards the end of their lives.”