Imagine that it is the week before finals. Think about those long hours cramming in Mugar Memorial Library where your sleep-deprived brain begs for just another jolt of caffeine. Leaving your books and notes behind, you walk to Starbucks and wait patiently as a mess of jumbled numbers and letters clutter your brain. Many people half-jokingly wish they had a coffee IV drip to automatically regulate caffeine levels during finals time — such a clever invention could minimize an overachieving student’s time and energy spent.
New technology developed at Massachusetts General Hospital is an anesthesiologist’s equivalent to the automatic barista. Doctors and researchers have developed an automated system that measures and processes brain activity, and it responds almost instantaneously with the necessary anesthetic.
The system was designed as a real-time feedback loop for intensive care unit patients who were induced into comas. Researchers believe this could eliminate some inefficient medical processes by replacing routine nurse checkups with constant monitoring by a computer.
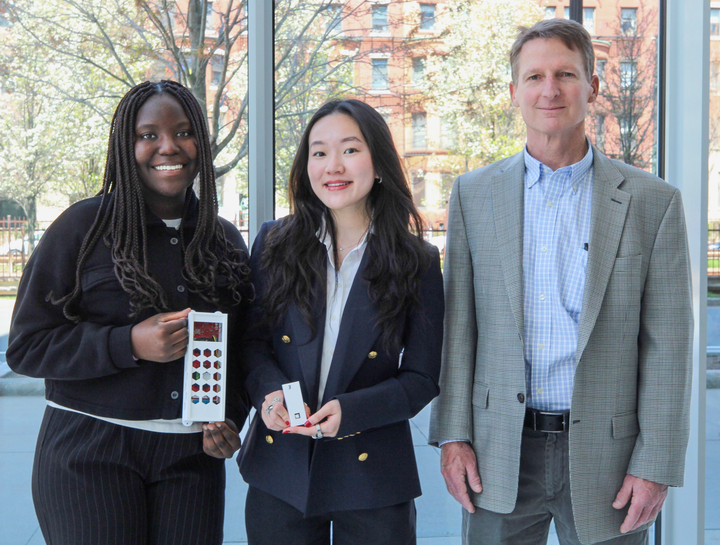
Emery Brown, the Edward Hood Taplin Professor of Medical Engineering at MIT, began designing this system about two years ago. According to a report in PLOS Computational Biology, the technology has already been tested in rats and has proven successful. Now, Brown and his team of MIT researchers plan to apply this technology to human subjects.
Brown said he designed this new system with induced coma patients in mind. People are sedated and put into comas for a number of reasons, including brain trauma from accidents and seizures.
“It [a coma] allows the brain to relax or rest and to let the swelling to go down so the injury can heal and the person can recover,” said Brown. “Or it’s used as a way to shut the brain down in patients who have epilepsy.”
The controller
The computerized care of the patient is determined by his or her electroencephalogram (EEG) pattern, which is the transmission of electrical waves from the brain. EEG patterns are different in conscious and in comatose patients. When awake, one’s brain activity is random, but within a narrow range. During a coma, however, brain activity is quiet with periodic bursts. The job of attending nurses is to control the number of these bursts, or the level of sedation. Burst suppression is crucial in the patient’s healing process because it controls the pressure buildup within the brain. Using anesthetics such as propofol, patients are kept at an optimal level of brain activity to allow the brain — and, of course, the patient — to properly rest and recover.
“The EEG is measured to see if you’re in that state,” Brown explained. “If you’re above that state, you might want to increase propofol. If you’re below that state, you might want to decrease propofol.”
The EEG is recorded using electrodes attached to the patient’s scalp. These are then connected to a computer, which responds by releasing the correct dosage of propofol through a connected infusion pump. This entire system combines the tasks of checking the EEG, determining the necessary dosage and administering the anesthetic into one simple and instantaneous step, a system Brown refers to as “the controller.”
“That’s what the controller tells the infusion pump to do — every second, it makes the decision about how to change the infusion rate,” added Brown.
Brown said he and researchers accomplished this using a computer algorithm based on common anesthesia procedures. Anesthesiologists know how to control brain activity using drugs and do not need a computer to calculate the correct dosage. However, this technology simply does the job for them, becoming the patient’s personal anesthesiologist 24 hours a day.
Brown compared induced comas to a trip to the moon. He said both can last for at least a couple of days and the procedures, from beginning to end, are highly predictable. The difference is that astronauts let the autopilot do all the work, while doctors work inefficiently.
“The autopilot tells you where to go, but you have to keep your hand on the control for three to five days [in space travel],” he said. “Nobody actually does that, but that’s essentially what’s happening in the ICU now.”
In addition to the autopilot function, the controller can be used to quickly increase or decrease the depth of the coma, depending on what doctors deem necessary. Overall, researchers believe the controller will use less anesthetic, which is both cost effective and healthier for the patient.
Traditionally, anesthesiologists have monitored patients using vital signs, including heart and lung activity. It has only been within the last year that doctors have relief on EEG for maintaining anesthesia and understanding its effects. A March news release from MGH highlighted a study that used EEG to measure consciousness in patients under propofol sedation. Brown was the senior author for this research.
Other systems measure EEG on a 100-point scale, and often aim to keep brain activity within a certain range, but Brown said “the controller” is much more exact. Precise sedation monitoring using EEG is what sets this controller apart from similar systems, he explained.
“Those that are being used, if they are, have not achieved the level of control that we have,” he said.
Although the controller has only been previously tested in rats, Brown and his colleagues hope for FDA approval to test the system in humans. They have also applied for a patent for their technology. Brown believes the system could be adjusted for use beyond just the ICU.
“Eventually, it could be used in the operating room, particularly for surgical cases lasting for many hours,” he added.
The outlook
Utilization of the computerized anesthesiologist could also promote overall staffing efficiency in hospital ICUs. Instead of monitoring comatose patients, whose conditions are critical but predictable, medical professionals could turn their attention to emergency situations that require doctors’ immediate skills or judgment.
During a long surgery, the system could eliminate the need for someone to monitor the anesthesia, creating more time, space and energy for doctors and nurses to focus on the surgery itself.
Cutting-edge technology is often expensive, especially in medicine, but it also means potentially paying nurses and doctors less.
Skeptics, however, may feel uneasy about replacing doctors with computerized systems and could point to statistics that show how a high percentage of hospital errors are caused by technology mishaps. Tom McTigue, a College of Arts and Sciences sophomore, said he is worried that medical technology, generally speaking, is susceptible to these types of errors.
“Machines are more efficient at handling the situation, and they can handle it faster,” McTigue said. “But if there was ever an error for the machine, it could be deadly for the patient.”
When Sedasys, Johnson & Johnson’s robotic anesthesia system, was approved in May, critics argued that hospitals still need trained doctors present to handle unforeseen medical emergencies. Sedasys is intended for colonoscopy patients and can completely eliminate the need for an anesthesiologist. While Brown’s continuous care system would not replace anesthesiologists entirely, the technology could face similar criticism to Sedasys.
In general, other critics of these “robotic doctors” fear that computerized care takes the element of personal human contact out of medical treatment. College of General Studies freshman Abbi Erkes shared similar feelings in regards to computerized medical care.
“There’s more room for error [with these technologies],” she said. “There’s less of a one-on-one level, or a patient-doctor relationship in which [treatment] can be more precautious, detailed-oriented and careful in life-or-death situations.”
After all, robots cannot reassure worried families and they are certainly not capable of having a doctor-patient relationship. As with all technology, human beings can never totally be replaced. Every field, especially the medical field, will always need trained people trained who understand concepts and who can provide that human element.
However, in the case of Brown’s controller, error has been proven rare because the brain’s activity patterns are so predictable and well understood by anesthesiologists and doctors.
We live in a world of real-time feedback loops, from global positioning systems to computerized fitness bracelets. The controller is another example of technology gathering an input — in this case, the EEG — and providing the needed output, being the propofol. Furthermore, it does it in a way that makes the overall job of nurses and doctors easier and more efficient, as most cutting-edge technologies tend to do.
But, like it or not, finals week will be here in just a few short weeks, and we’ll still be making coffee runs the old-fashioned way.
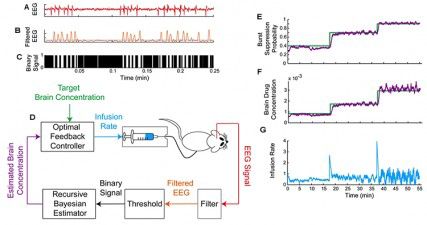
Panel A shows raw EEG recorded in burst suppression. Panel B shows the filtered EEG with the threshold. In Panel C, based on the threshold, the filtered EEG is converted into a binary signal: 1 below the threshold and 0 above the threshold. The control scheme is shown in Panel D. The target brain concentration of propofol (green) is input to the controller, the infusion of propofol from a syringe pump is initiated by the controller and propofol is infused into the rat. The EEG is recorded continuously, filtered, thresholded and converted into a binary signal in real time. In real time the Bayesian estimator determines the estimated brain propofol concentration (purple) based on the binary signal. The controller compares the estimated brain concentration with target brain concentration and updates the infusion rate of the pump accordingly. The updates occur on a one-second time scale. Panels E-G show the experimental results from a one-hour run of the controller. The target propofol concentration (Panel F, green line) or equivalently the target burst suppression probability (Panel E, green line) was set at 0.4 for 18 minutes, then at 0.7 for 20 minutes and finally at 0.9 17 minutes. The burst suppression probability is the instantaneous probability of the EEG being suppressed. The controller achieved and maintained the target burst suppression probability (Panel E, purple curve, estimated burst suppression probability), or equivalently, the target brain drug concentration (Panel F, purple curve estimated brain drug concentration) accurately and reliably across all three levels. Of particular note, the controller was able to make vertical climbs between levels without overshoot. Panel G shows the instantaneous infusion rates used by the controller to achieve and maintain the targeted level.