From newspapers and television to Twitter and word of mouth, 2014 has been saturated with news over the rare and infectious Ebola virus. Most recent is the case of Kaci Hickox, a Maine nurse who was isolated for three days following her return from Sierra Leone on Oct. 24 and, even after exhibiting no symptoms, was ordered to remain quarantined in her home by state health officials for a 21-day incubation period, an order she successfully overturned in court on Friday.
As of Wednesday, there have been 13,703 cases of Ebola reported, and 4,920 people have died because of the virus, according to the World Health Organization.
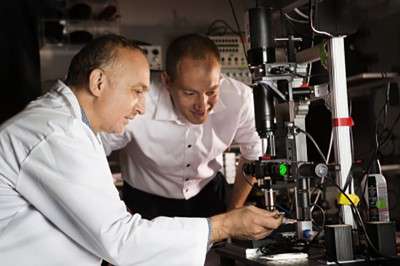
As a call to action, the disease’s current outbreak in West Africa has spurred both conversation and research on fighting against Ebola, including a prototype shoebox-sized device created by several Boston University and University of Texas Medical Branch professors.
Single particle interferometric reflectance imaging sensor (SP-IRIS) combines LED and nanotechnology to provide what many believe is the root need of Ebola-stricken populations: a means of efficient detection, said Selim Ünlü, lead researcher and professor of biomedical, electrical and computer engineering at BU.
“The most common traditional method [of detection] is PCR [polymer chain reaction], which typically requires significant sample preparation and expensive equipment,” he said. “We can work with a blood sample with minimal processing.”
PCR can take up to three hours per detection, Ünlü said, while the current SP-IRIS prototype only requires an hour, at most, to deliver results, providing a significant advantage over the time-sensitive effects of infectious disease.
Along with efficiency, the cost of diagnosing Ebola is another problem that faces traditional detection methods. Ünlü said further models of the SP-IRIS instrument could have a low cost in mass production.
“The fundamental problem is that the health care systems where Ebola has been are not strong and haven’t been able to keep up with the sudden demands placed on them,” said Malcolm Bryant, a clinical associate professor of global health at the BU School of Public Health.
But how does SP-IRIS work? The device “shines light” on Ebola, Ünlü said, by exposing viral particles on a sensor coated with antibodies by way of LED light.
“The sensor surface is very large and can capture the telltale responses of up to a million nanoparticles,” Ünlü said. “Thus, the viruses on the sensor surface are counted in a digital detection modality.”
While the operational mechanics of the device may seem complicated, its aim is to streamline a process that has a difficult time of keeping up with viruses such as Ebola that can infect a population quickly.
The device, which has been five years in the making, is being tested at several labs at UTMB and at the BU Photonics Center. Ünlü said his team hopes the tool will be put to use by patients and medical professionals in two or three years.
“The opportunity to be able to do a rapid diagnosis of Ebola onsite would greatly aid the workers in the field and the patients suffering from the symptoms of the virus,” Bryant said.
The rate of new Ebola cases, which saw almost 1,000 new cases during the week of Sept. 14 to 20, according to the WHO, has shown the world that new methods of diagnosis will be key to handling future outbreaks, Bryant said.
“If you have a test that can avoid a two to three day wait for diagnosis and the beginning of treatment, you would enable them [patients] to no longer be a burden [on healthcare operations], and they can leave,” he said. “This can help them avoid contracting the disease, and that can be only a benefit.”






































































































M Mukunyadzi • Nov 6, 2014 at 10:03 am
They need to try this on Humans ,this is needed fast .