
Even after conquering tumors, cancer patients are often still plagued by fatigue. This exhaustion creates a barrier for those seeking a return to their regular lives.
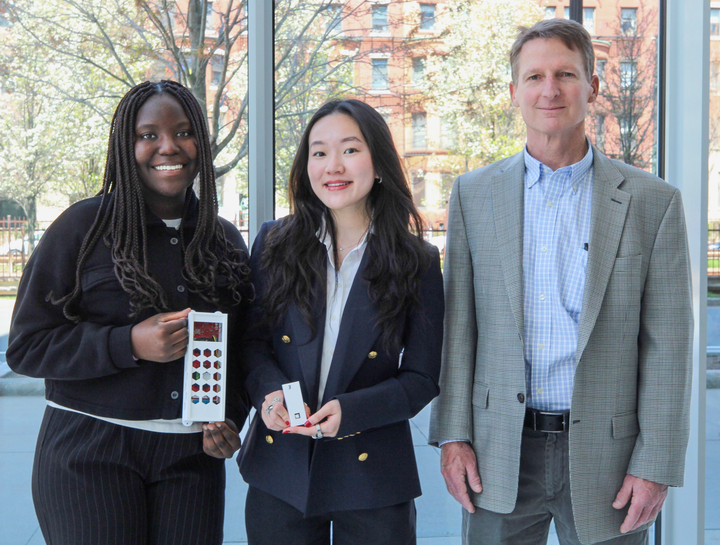
In a study released earlier this month, researchers at Harvard Medical School partnered with researchers from the University of Alabama at Birmingham and discovered that administering placebos, even with full disclosure, correlated to a decrease in fatigue.
“If you go to a horror film and you have a physiologic reaction, you know it’s not real and yet you have that response,” said Dr. Kevin Fontaine, chair of the Department of Health Behavior at UAB’s School of Public Health.
Fontaine and Dr. Teri Hoenemeyer, a scientist at UAB’s Comprehensive Care Center, spearheaded the study. Hoenemeyer’s said interactions with patients undergoing end-of-life care spurred her interest in the study.
“After practicing yoga or meditation, [patients] were saying that they felt better, that they could perform more activities,” she said. “Even when they were within a couple of weeks from the end of life … they still felt like these therapies were helpful to them.”
From this, Hoenemeyer developed an interest in the placebo effect as a way of trying to explain what might be going on physiologically during these therapies.
“Fatigue is [cancer patients’] number one complaint. It seems to last not only through treatment, but also long after treatment ends,” Hoenemeyer said. “It is the most distressing [symptom] that patients say they have after treatment because it impacts their social activities and work life.”
Hoenemeyer said that she wanted to investigate how to alleviate their tiredness without the onslaught of side effects traditional medications can impose.
The 74 individuals used in the study, all cancer survivors, were randomly assigned for 21 days to either the “open-label placebo” group, placebo pills with full disclosure, or the “treatment as usual” group, which had minimal or no medication.
According to Fontaine, individuals resided in five rural and urban counties surrounding the university, with nearly a quarter African American people. “It was the first open-label placebo study that had that many African Americans,” Fontaine said.
Fontaine explained that participants received placebo orientation before being randomized into an experimental group.
“We primed them to learn about the placebo effect and to at least potentially be willing to try it,” he said.
The results, Fontaine said, showed no correlation between a participant’s belief in the placebo’s success and its shown effect. “[This] adds layers of fascination and confusion about what’s going on for me,” he added.
Annie Heyman, a sophomore in Boston University’s Seven Year Liberal Arts/Medical Education Program, has learned about the placebo effect in several classes. As a future medical professional, Heyman said she is intrigued by the results of the study.
“If you can tell your patients up front that what you’re giving them is not actually going to do something or not expected to do anything, that’s amazing … and more ethically acceptable.”
When asked about the mechanism behind the success of the placebo pills, Hoenemeyer said the brain-body connection could play an important role.
“When someone takes a placebo, those areas of the brain light up as though it’s an active drug,” she said. “And those are the areas that help us feel better, help us not be so depressed, help us with pain management.”
Fontaine said the pill may have succeeded because of an expectation, even though participants knew it contained no active ingredients.
“We associate pill-taking with feeling better in a sort of classical, Pavlovian conditioning,” he said.
While the study’s results could have great implications for treating cancer patients, acquiring further funding to continue research has been difficult, Fontaine said.
“It has been very difficult to get funding because we haven’t really nailed down what the mechanisms are and that’s an issue because the effects are very large and it seems worthy of federal funding.”
Both researchers said they believe in the power of the placebo in improving patient care.
“We have a moral obligation to treat them and not just focus on curing,” Hoenemeyer said. “You treat the patient and not just the disease.”
Correction: A previous version of this article attributed the quote “[This] adds layers of fascination and confusion about what’s going on for me” to Hoenemeyer. It should be attributed to Fontaine. The current version reflects this.

























































































































Betty King • Feb 22, 2018 at 6:55 pm
Please make your next study for MS. Fatigue is one of the worst symptoms.
mona • Feb 23, 2018 at 1:31 am
My close friend has MS for many years now , and she works everyday as a dermatologist with two kids !! That’s really surprising ! just thought it could boost yoyr mood hopefully !