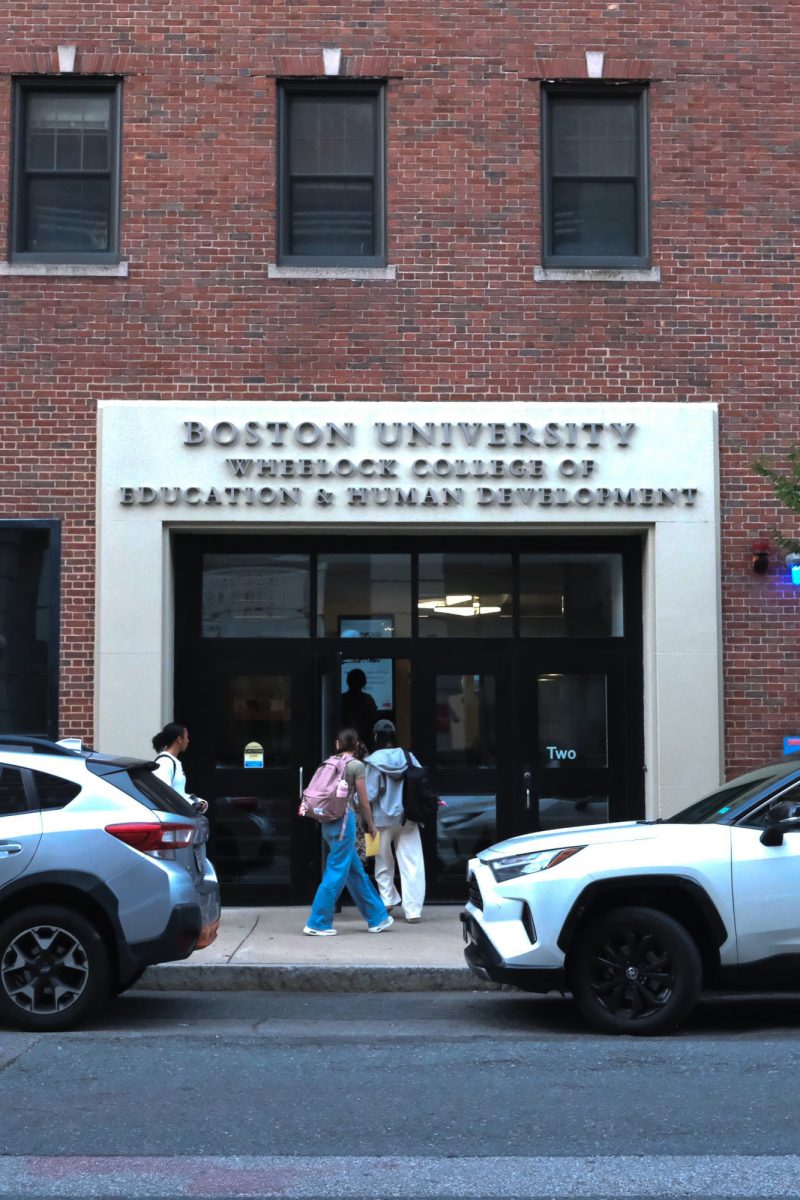
Researchers from Boston University and Harvard University created a model to better understand how human wounds heal.

By using an in-vitro model with human cells, scientists were able to replicate a portion of the wound closing process and provide insight into the dynamics of tissue formation for wound closure, which could have significant implications for future research on diseases and drug development.
The study, published in January, is a collaboration between BU’s Biological Design Center and Department of Biomedical Engineering, as well as The Wyss Institute for Biologically Inspired Engineering at Harvard.
BU College of Engineering Ph.D. student Juliann Tefft, ENG research assistant professor Jeroen Eyckmans and biomedical engineering professor Christopher Chen completed the research.
Tissue formation is necessary for wound closure, but up until the paper, researchers had difficulty understanding how different types of cells, namely endothelial cells and fibroblasts, interacted with each other to form such tissue.
Their model, described in the paper as a “three-dimensional, engineered vascularized human tissue” provides new insight into the process because the researchers were able to create a controlled environment for studying how the tissue forms.
Eyckmans said this work is crucial for understanding tissue regeneration.
He said the ultimate goal of this research is to create better models that capture human disease and human physiology. He added this model is a stepping stone toward developing treatments for wounds that don’t naturally heal due to various diseases.
“Diabetic patients and patients with neuropathologies, their wounds don’t heal well, and so we don’t have a good understanding as for why that is,” Eyckmans said. “[Once] we have a model system that works, then we can sort of trigger a disease in the model system, which will then have implications for drug discovery.”
However, Eyckmans said there are also limitations to the in-vitro system. For example, researchers expected the cells would send signals to attract blood vessels into the wound area, but this did not happen.
“We are still missing components in our model system, so that needs further exploration,” he said.
In-vitro models offer different insights compared to animal studies, Eyckmans said, which historically have been done in this field on mice, pigs, sheep, rats and dogs, according to Citizens for Alternatives to Animal Research and Experimentation — a nonprofit advocating for the elimination of animal testing.
However, he said having this in-vitro system allows for manipulating the environment in a more intentional and controlled manner, and this is different from studying with an animal model.
“The great thing about an in-vitro system is you have so much more degrees of freedom to manipulate the system and to learn from how cells behave without having all the other factors,” Eyckmans said. “In a in-vitro system, you can sort of isolate the things you’re interested in.”
With animal testing, Eyckmans said, “it’s always a much more complex environment to work in, with potential confounding factors,” such as different cell types.
Tefft said she was initially interested in this work due to its connection to differences in scarring after surgery. She said there are several conditions that prevent wounds from healing properly, such as diabetes, which the model could investigate.
“It might not be directly related to what’s happening in diabetes just yet, but [the model] could help us kind of put the puzzle pieces together,” she said in an interview. “We have a basic system that, if we keep on adding pieces into it, we can get a good idea of what’s going on.”
Like Eyckmans, Tefft said she thinks the current model is simple, and there is room for adding complexity and incorporating more elements.
“The way I see our model fitting into research right now is to study basic aspects of healing, where we can control exactly what is happening at any given time,” she said. “I’m hoping that our model specifically can help us understand what controls the growth of blood vessels into new tissue during the early stages of wound healing.”
Tefft said there is still a need in the industry for some animal testing to fully understand the healing process, but this human-cell model could potentially improve in the future.
“My hope is that, in however many years, maybe 20, maybe 50, we’ll have a model that is so complex using human cells that it’ll be super accurate to show how humans feel,” she said. “We’re not quite there yet, but I have hopes that we’ll get there one day.”