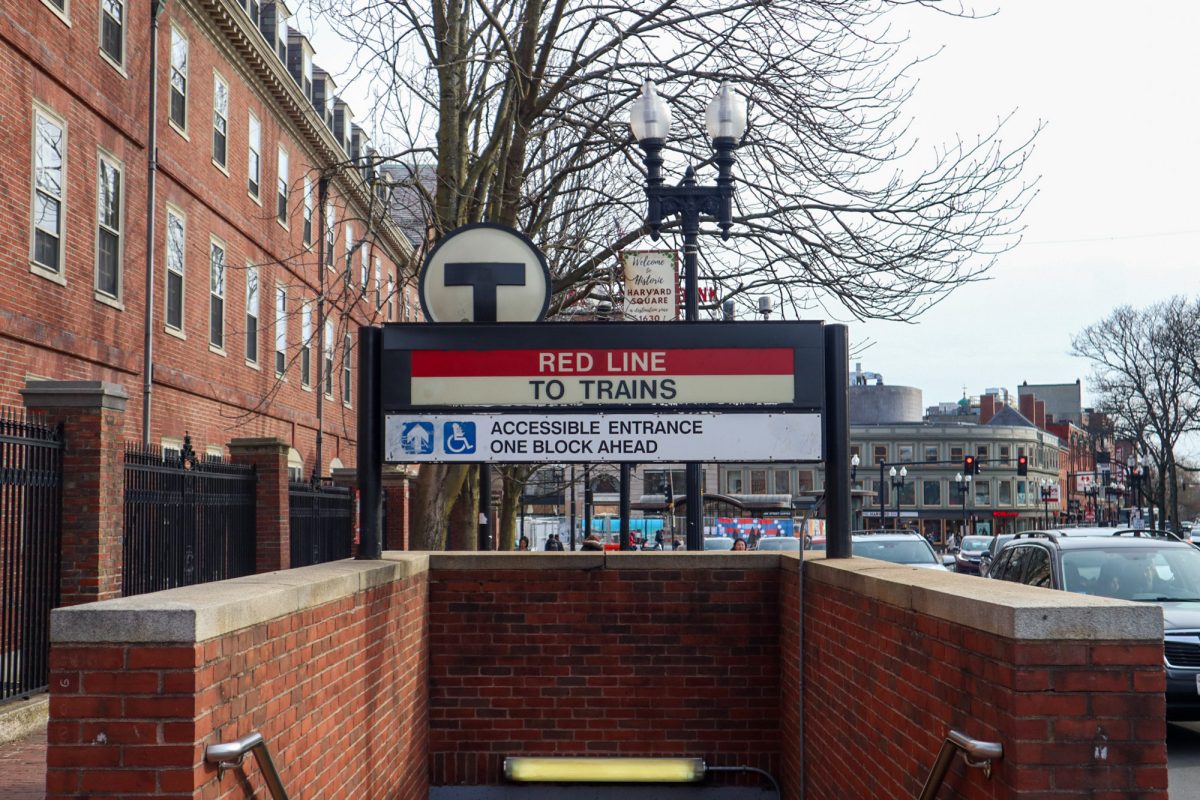
Three medical students at Boston University School of Medicine started a campaign and petition calling for hospitals to end the universal shackling of incarcerated patients, starting with Boston Medical Center. The petition, published Feb. 5, proposes a policy that would instead assess patients on an individual level to determine if, and to what extent, restraints are necessary.

Binding patients to hospital beds – with shackles or handcuffs attached to their wrists, ankles or waists – is a human rights violation, a medical ethics violation and harmful toward both patient outcomes and patient-provider relationships, said campaign directors Neil Singh Bedi, Nisha Mathur and Judy Wang.
Bedi said normally, for patients who need to be restrained, there are more comprehensive protocols to make sure that only the exact restraints necessary are being used, “no more, no less.”
However, almost all incarcerated patients are shackled, he said.
“The question involved for me was, ‘why don’t we do this with all of our patients, right?’ ” Bedi said. “We’re not saying that shackling or restraining patients isn’t necessary, there are times for it, but why don’t we have the same humane protocols apply to incarcerated patients as well?”
The decision to shackle all incarcerated patients at BMC is currently in the hands of the Department of Corrections, the petition said.
George Annas, a professor in the School of Public Health, said hospitals defer to prison officials on when to shackle patients for their safety and to prevent them from fleeing.
“The presumption now is that everybody’s dangerous, everybody’s going to escape, so we have to shackle everybody,” Annas, who also helped with the campaign and signed the petition, said. “The students think that the presumption should be everybody should be treated individually.”
BMC’s policy is to not shackle incarcerated pregnant patients following an earlier movement that led to the implementation of a 2014 Massachusetts law that banned perinatal shackling, the petition said.
“Women who are giving birth, they’re not escaping anywhere,” Annas said. “They’re having a baby.”
The campaign aims to extend this to all incarcerated patients and believes this is an “excellent foundation” in doing so.
Sondra S. Crosby, a professor of medicine at Boston University and a physician at BMC, wrote in an email that she has witnessed countless times healthcare professionals and institutions – including herself in the past – turning “a blind eye to the practice of shackling incarcerated patients, even while they are dying.”
“Incarcerated patients are arguably our most vulnerable population, and deserve to be protected and treated with humanity, not deprived of it,” Crosby wrote.
Bedi said, as a medical student, he has witnessed scenarios in which no one questions harmful standards.
“We see things in the hospital and we’re just like, you know what, that’s how we do things,” Bedi said. “That’s just how the way things have always worked.”
Crosby, who also helped with the campaign and signed the petition, said part of what makes the practice so inherent in medicine is its history, which is riddled with racist undertones.
“Shackling conjures the image of shackled slaves, and has been used historically until present day as a method of torture, cruel, inhuman, and degrading treatment,” Crosby wrote.
An employee of BMC, Tyler Lescure published an op-ed in the Washington Post describing his experience caring for a shackled, incarcerated black man at the center who was critically ill and in a medically induced coma, and died while still shackled.
The “visible presence” of shackles on patients of color – who are overrepresented in the incarcerated patient population – can reinforce racial bias and oppressive attitudes, which then worsens the patients’ health outcomes, Bedi and the petition said. The petition said hospital policy should not worsen the greater mistrust that people of color already have of healthcare workers.
Annas said hospitals are likely concerned about liability.
“A dangerous prisoner is going to hurt another patient, then that patient is going to sue the hospital,” Annas said. “That’s why they just say, let the sheriff take care of that, or the warden.”
Mathur said the first step in building the campaign was a “giant literature review” in order to educate themselves on the issues at hand.
“The patients whose voices we’re hoping to amplify are already disenfranchised,” Wang said. “They are already very vulnerable and to place a burden on them to educate us, I think, isn’t appropriate and so I want to be respectful of that.”
Crosby believes legislation is the only way to end the issue, and that a solution would require input from many stakeholders, including the Department of Corrections.
But Wang said although social change and healthcare reform is difficult to enact, the directors of the campaign remain hopeful that BMC can reform its policies, recognizing the hospital for “their incredible work achieving Health Justice already.”
“Boston Medical Center has done hard things in the past,” said Wang. “They’ve demonstrated a great response to the pandemic … we believe that they can continue to do hard things moving forward.”