Two Boston University researchers received a grant to model how “Medicare Part B” payment policy affects the price path of physician-administered drugs. The grant was awarded by the National Institute for Health Care Management Foundation (NIHCM).

“Medicare Part B” offers two types of services — medically necessary services and preventive services — according to medicare.gov. Under the current United States pharmaceutical payment system, physician-administered drugs, including treatments for serious illnesses such as cancer, are included in Medicare Part B.
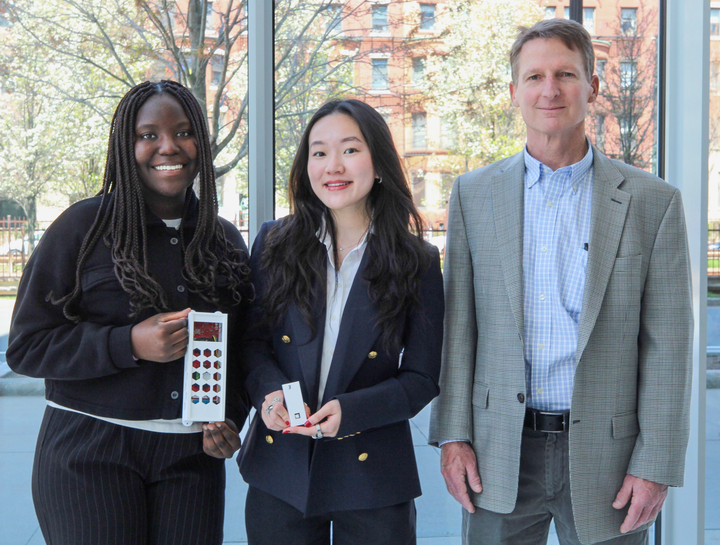
Keith Ericson, associate professor of markets, public policy and law at Questrom School of Business, and Angie Acquatella, postdoctoral fellow at Questrom, are aiming to study the “optimal design of financial incentives and health care” along with their research colleague, Amanda Starc from Northwestern University
“I’m really interested in designing systems so that people make good choices about using resources and getting the best health outcomes possible,” Ericson said. “The decision [of drug using] I think, is made jointly between the physician and the patient, but the physician has a big financial incentive to prescribe the higher-priced drugs.”
The current payment system produces “a conflict of interest,” Christopher Robertson, professor of Law and N. Neal Pike Scholar in Health & Disability Law at BU, said.
“Medicare Part B is for a peculiar class of drugs that the physicians actually dispense and administer themselves,” he said.
Robertson explained how physician-administered drugs are typically ones that have to be injected or infused. The physician is the one who actually purchases the drugs, then they resell them to patients.
“If that reimbursement system is not designed appropriately, it could cause physicians to select drugs for their patients that are either more expensive or less effective than they ideally would be,” he said.
Acquatella said her goal is to understand how the way the government pays for physician-administered drugs affects their “pricing dynamics and treatment outcomes.” She said that measuring how physicians “internalize” financial incentives is helpful to “inform better design of how to pay for these inputs to care.”
“The overall research agenda that I have focuses on how the way we structure financial incentives affects who receives care and what kind of care people receive,” Acquatella said.
Ericson and his team are investigating a variety of data, including changes in reimbursement rates, to build a predictive model on “Medicare Part B” pricing. Using the model, Ericson hopes to evaluate the potential impacts of alternative payment policies on physician-administered drugs.
“My dream would be recommendations for how to redesign and pay for these types of drugs,” Ericson said.
While Ericson’s team focuses on economic modeling, Robertson’s research centers on the “bioethics of conflicts of interests and behavioral science.” In 2019, he published a book called “Exposed: Why Our Health Insurance is Incomplete and What Can be Done About It,” in which he suggested that healthcare cost exposures are inefficient, particularly through the “co-pay” system.
Robertson said that although patients are exposed to the costs of their treatments, they are “often not in a position to really make a healthcare decision,” as Ericson’s research shows.
“It doesn’t really make sense to make the patient have to pay out of pocket when truly the physician [is] making the decision,” Robertson said.
Ericson and his team are using the grant to address this problem by proposing alternative payment policies that Medicare and commercial insurers might adopt for physician-administered drugs.
“The grant really gives us the resources we need to do the work, so I mean, acquiring data, helping support staff time, and travel to conferences,” Ericson said. “To get this out in front of policymakers when we get to that stage.”
Ericson said that the Undergraduate Research Opportunities Program is a potential channel for undergraduate students to get involved in similar projects. Given that his research topic is both policy-relevant and scientific, Ericson said that this study can help the community understand how public policy is informed by research.
The research is made to help inform the “patient side of the market,” Acquatella said.
“Within the BU community if anyone suffers a condition that requires physician-administered
drugs, or has a family member that is going to the doctor and going through this process of which chemotherapy regime they choose then this is informative,” she said.