As the world’s technological landscape rapidly evolves, innovations once thought unimaginable are drastically transforming the ways in which we live.
One such innovation, virtual reality, is typically viewed as a means of entertainment and, more specifically, a gaming console. However, this phenomenon also has extraordinary applications within the field of science that could benefit us in extraordinary ways.
In recent years, institutions across the globe have begun researching how virtual reality could be utilized in mental health services, said Hayley Fitzgerald, a postdoctoral associate at Boston University.
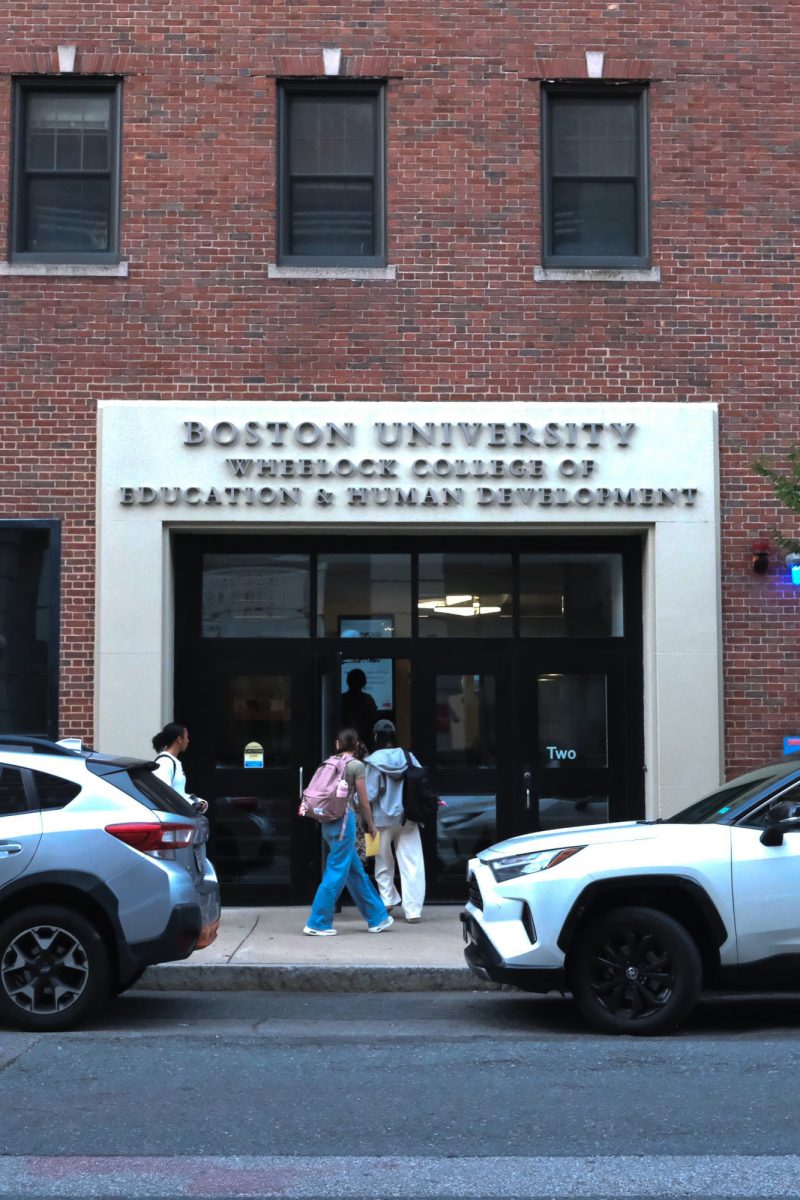
At BU, several studies that examine how virtual reality could be used to alleviate anxiety, phobias and even nightmare-related disorders have emerged.
A handful of studies are being conducted at BU’s Center for Anxiety and Related Disorders. Fitzgerald, along with Laura Long, another postdoctoral associate at the center, are working on a study relating to VR interventions for speech anxiety.
For this study, Fitzgerald said, they are exploring variables that may impact the effectiveness of virtual reality in treating patients with speech anxiety.
Although BU is the lead site for this research, this study has taken a collaborative effort that includes 14 other sites across the globe, as part of an international research community called the Exposure Therapy Consortium, said Long.
Long said she is also working on a study using VR intervention to address the fear of heights, which is currently recruiting participants.
“We can’t necessarily have people go up to a mountain, but we can bring the mountain to you with the VR technology and help people engage with the image of heights in a way that’s very safe and controlled and feels pretty real,” Long said.
In 2019, two BU professors — Patrick McNamara, associate professor of neurology, and Wesley J. Wildman, professor of philosophy, theology and ethics and of computing and data sciences, joined forces to conduct a pilot study investigating how different treatments could be used to alleviate the distress associated with nightmares, Wildman said.
For this study, they used what is known as a rescripting protocol to reduce the intensity and “dominance” of images in nightmares, said McNamara.
“When an image is dominant, it controls your emotions and attention,” he said. “There’s a lot of evidence that that’s a big factor in creating the distress associated with nightmares.”
When research first began, there were two primary pre-existing methods, said McNamara.
The first, he said, is called imagery rehearsal therapy, which uses the rescripting protocol. However, the problem is that it requires months to take effect and it does not work for everyone, he said.
Additionally, these traditional methods run the risk of retraumatizing patients by having them imagine the same images that scared them in the first place, Wildman said.
The alternative to this is drug therapy, which often has serious side effects, said McNamara.
“We were looking for a way to treat nightmares and distress associated with nightmares that was better than the standard imagery rehearsal therapy and could rival the drugs used to treat nightmares,” he said. “We could train people to reduce the dominance associated with images with 45 minutes or so of viewing dominant images and re-scripting them.”
Through virtual reality technology, researchers provided participants of this study with dominant images, like a shark or a gun, for instance, and had participants redraw them into something that appeared less threatening.
They found that participants who did this a few times a week experienced reduced distress associated with nightmares, he said, but even reduced general anxiety as well.
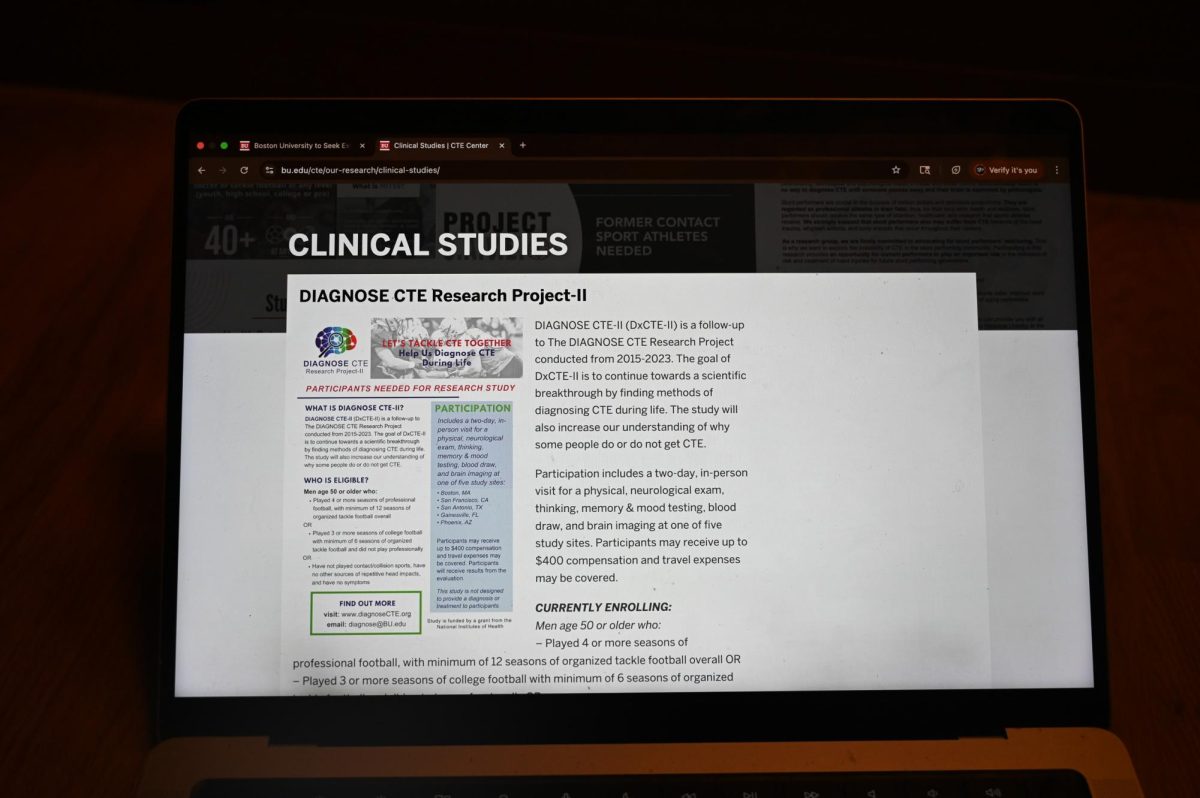
Now they are proceeding to the next step, a double-blind clinical trial, but McNamara said they are facing issues receiving sufficient funding.
A double-blind clinical trial is a study that evaluates the effectiveness of a medical treatment, but neither the researchers nor the participants know which treatment the participants are receiving until the trial ends.
VR technology will likely become more prominent within mental health services in the future, Fitzgerald said.
“If you look at older research studies that used VR, sometimes the images that our patients were looking at really don’t look real,” she said. “I think now the technology is improving so much that, when we’re in these situations with the VR headsets and we’re helping our patients’ approach, it can feel pretty real.”
Evan Thompson, president of the MIT Virtual Reality/Augmented Reality Club, said the technology still has ways to go.
VR’s hardware has significant limitations, as it requires headsets to always be tethered to external power sources, restricting the user’s mobility and comfort when using the device, he said. Additionally, some people may experience motion sickness when using virtual reality.
Despite these technical issues, McNamara said he anticipates VR being a transformative technology for mental health treatments.
“The promise of virtual reality for transforming experimental approaches to mental health issues is immense,” McNamara said. “Progress has been rapid, and I anticipate much more progress in the near future.”