A new device developed by a Boston University professor and research team can determine whether or not an antimalarial drug will work.
The buzzing of a mosquito is never a welcomed sound. In developed countries, the insects are often the uninvited guests at summer picnics, pool parties and nature outings. The red, itchy bites a mosquito leaves on the skin of its victim will keep the person scratching for days.
However, in the underdeveloped tropical and subtropical areas of the world, the sound of a mosquito takes on a more ominous tone. A single bite from a female Anopheles mosquito carrying the malaria parasite is enough to infect a person with the potentially deadly disease. While malaria is treatable, with ineffective anti-malarial drugs running rampant throughout developing countries, a mosquito bite can easily become a death sentence.
Muhammad Zaman, associate professor of biomedical engineering at Boston University, has been working to address the problem of ineffective drugs in the developing world. In early 2012, Zaman received a two-year grant for $250,000 from the organization, Saving Lives at Birth, to develop a device with the capability to determine the effectiveness of a drug.
“One of the biggest challenges in the developing world is not just the availability of medicines, but the availability of good-quality medicines,” Zaman said.
A COSTLY PROBLEM
The early stage of malaria manifests as symptoms easily confused with symptoms of the common cold or the flu, according to the Centers of Disease Control and Prevention website. A victim will experience the chills, a fever, nausea and sweats.
Without the proper treatment and care, the disease can take a dangerous turn and lead to low blood pressure, acute kidney failure, acute respiratory distress syndrome (ARDS), severe anemia, cerebral malaria and death.
Malaria is the fifth-leading cause of death from infectious diseases worldwide and the second leading cause of death from infectious diseases in Africa, following HIV/AIDS, according to the CDC. About one million people living in tropical and subtropical areas die from malaria each year, and 89 percent of those deaths occur in Africa.
Many of these deaths could have been prevented if not for, as estimated by the World Health Organization, the 30 to 40 percent of all antimalarial drugs that are currently ineffective.
Zaman said the anti-malarial drugs become ineffective for numerous reasons.
Counterfeiting, an illegal activity in which the drug may be contaminated or not contain the correct ingredient or the correct dosage, accounts for about one-third of the ineffective antimalarial drugs.
However, fewer malicious acts such as poor production, improper storage or a general lack of awareness of the proper procedures involved in handling the drugs and administering them to the patient can result in low quality drugs, Zaman said.
Zaman estimates that the cost of these counterfeit or substandard drugs amounts to about $70 billion each year.
Even worse, ineffective drugs today can lead to serious ramifications that the future generation will have to address.
“The problem is not just immediate financial burden or immediate loss of life or increase of sickness. The effect is very, very long term,” Zaman said. “We start to see resistance against drugs. Our arsenal against deadly drugs starts to shrink, and it’s a problem. It’s one of those white elephants in the room where everybody knows what it is but really nobody pays any attention to addressing this huge, huge challenge.”
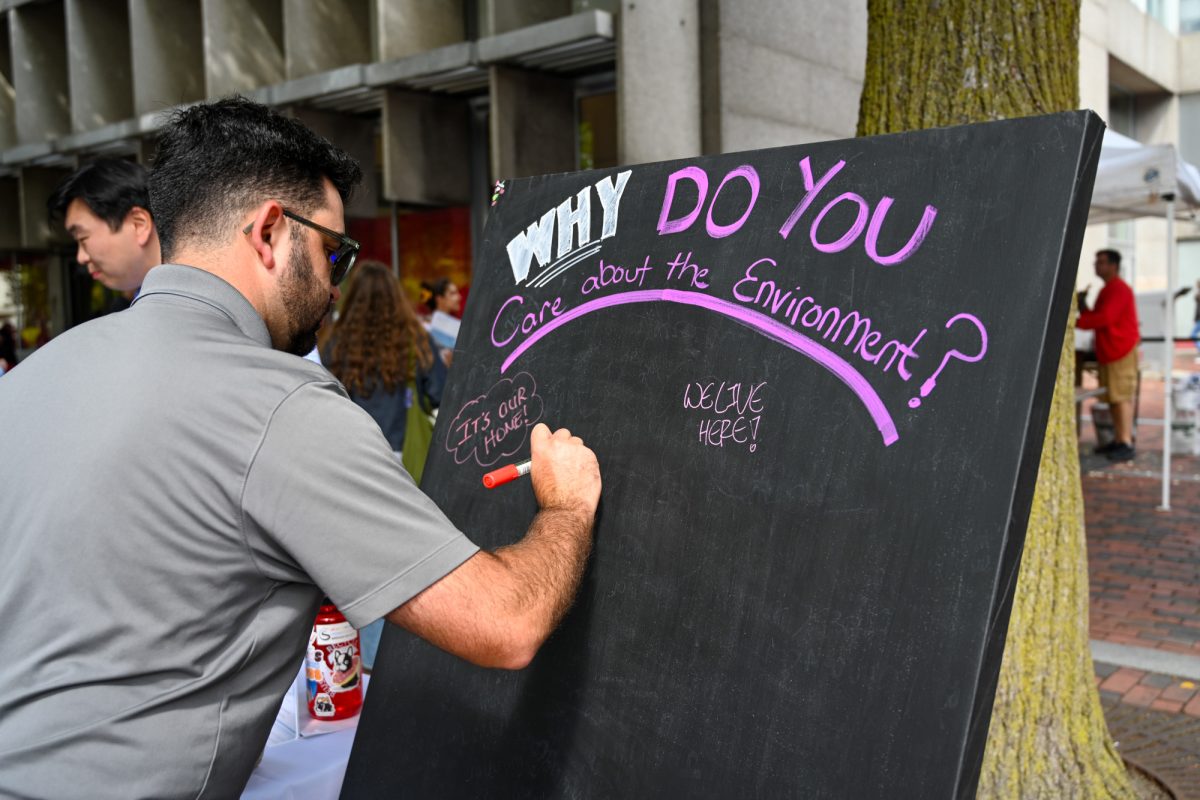
Many BU students said they are surprised by the extent of this little-known problem.
“Here in the United States, we just assume that the drugs we get will work,” said Gabriella Vassil, a sophomore in the School of Management. “But I realize that’s not the case in underdeveloped countries.”
“It’s almost scary how easily this topic can be overlooked,” said Kaitlin Walsh, a sophomore in the College of Arts and Sciences. “I think that most people probably don’t even know the problems that ineffective drugs are causing, or at least they think it won’t affect them. But the reality is that this could become a major issue for the entire world.”
SIMPLE SOLUTION
While current methods of testing the effectiveness of drugs exist, these methods are often too expensive or complicated for developing countries. Having grown up in Pakistan, Zaman is highly aware of the health hardships and needs that people living in developing countries face everyday.
“[Developing countries] require simple, affordable, robust and scalable technologies that can solve the problems of people who do not have a dollar a day to live off of,” Zaman said. “Addressing those types of concerns requires creativity and engineering ingenuity. We can have the coolest technology, the best gadget to deliver the drugs and deliver the medicine, but if the drug itself is problematic, if it’s compromised, then it doesn’t do anything,”
Zaman and his team designed the device to be easily employed in developing countries, which includes a library of probes that quantify the amount of the drug, the concentration of it and how it should dissolve appropriately.
The device itself weighs fewer than 10 lbs. and consists of a pump, some tubing and a small microchip. It will work in tandem with any type of smartphone “that has the capacity to do basic imaging and analysis,” Zaman said.
“I think it’s really cool that researchers are developing technologies that work with smartphones,” said Casey Cirillo, a CAS freshman. “It’s so practical because they are relatively simple to use and almost everyone has one.”
FURTHER AND FUTURE APPLICATION
Zaman said he foresees that the device will have many uses in the future.
“We see it being used at multiple levels and multiple angles. We envision it being used for regulatory purposes, to ensure that quality control standards are met across the various levels of supply chains in a given country, in a given developing country,” Zaman said. “They have many cases of poor-quality medicines leading to massive loss of life and financial impact.”
Zaman noted that the device could benefit small pharmaceutical companies who wish to ensure that quality control standards are achieved and for smaller hospitals and clinics lacking the capabilities and technologies of large scale infrastructure.
The device will also be able to test the effectiveness of other types of drugs, such as tuberculosis and other infectious diseases.
It is technology such as Zaman’s device that holds the key to improved overall health and fewer preventable deaths worldwide.
“It’s great to hear about the cutting-edge technology being developed right here at Boston University,” said Lisa Fredrickson, a junior in CAS. “It makes me extremely proud to be a student here. The work of our professors and students is making a difference.”