Healthcare workers and advocates, including a Boston University public health professor, testified before the Massachusetts Joint Committee on Public Health in a Monday hearing at the Massachusetts State House.

The hearing discussed two proposed bills: Bill H.2469 and Bill H.2534, which aim to preserve access to essential health care in response to more than 40 closures of hospitals and hospital services since 2009.
Alan Sager, professor of health law, policy and management at BU School of Public Health, was among those who testified. Sager used his expertise and years of research on health care reform to emphasize the importance of the proposed bills.
“Health care is governed by anarchy. Nobody’s accountable for anything,” Sager said in an interview with The Daily Free Press.
In his testimony at the hearing, Sager said these “bills begin the job of boosting accountability.”
Members of the Massachusetts Nurses Association also testified at the hearing.
Despite the Department of Public Health finding that services at more than 40 Massachusetts hospitals were “essential to preserving access and health status in the community,” those facilities still closed, according to the MNA.
Katie Murphy, president of the MNA and an ICU nurse, testified the closure of health care services throughout the state is a “crisis.”
“Decisions about these closures are made in boardrooms against the best interests of patients and their communities who suffer without local, clinically appropriate care,” she said.
Bill H.2469 would require hospitals preparing to discontinue services to show proof that they sought and received community feedback at least a year before filing an intent to close with the state.
The bill would also require hospitals to allow for commentary and objections by affected municipalities, prevent hospitals that close essential health services from opening new health services for three years and block the closure of any hospital facilities during a state of emergency.
“It will slow down efforts to close hospitals and expose them to greater public scrutiny,” Sager said. “It will also permit and invite greater participation from citizens who are affected by [the] closing.”
The second bill, H.2534, would create a process for state receivership of hospitals that discontinue healthcare services despite those services being deemed essential. State receivership is a legal process that places a financially distressed but essential health care facility under the control of a neutral third party.
Murphy said the closures are driven by “profits over patients.”
“We see the essential services for the community being closed and higher reimbursement services put in place,” she said.
Health spending in the U.S. increased by 7.5% in 2023 to $4.9 trillion, and continues to rise every year, according to the American Medical Association.
Sager said the rising costs is especially a problem in Massachusetts, given the state’s health care is “just about the most expensive in the world,” he said in the interview.
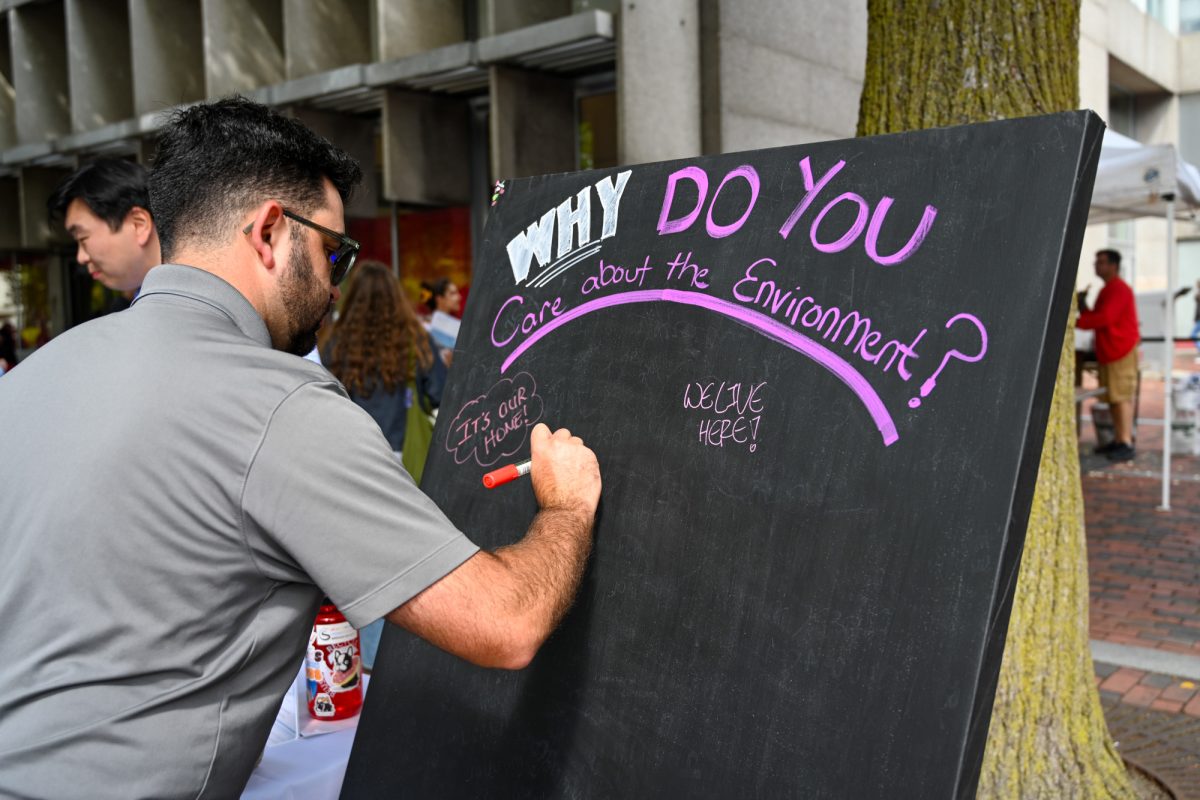
“That sponges up money that isn’t available for the environment, education, job training, rebuilding, manufacturing, defense, housing, nutrition and all the other things people care about,” Sager added.
Murphy said the section of the bill preventing hospitals from opening a new health service for three years after closing could discourage financially motivated shutdowns.
“We just are hoping that this puts some teeth into [the law], so that hospitals will reconsider and say, ‘Three years down the road, maybe we’ll keep this open,’” she said.
Joe-Ann Fergus, director of MNA’s Division of Member Services, emphasized the harmful community impact caused by closures of two full-service hospitals in Ayer and Dorchester, as a result of Steward Healthcare’s bankruptcy filing last year.
“In that time, [Steward Healthcare] oversaw the closure of numerous maternity, pediatric and behavioral health units … leaving already vulnerable communities without access to essential health services,” Fergus said.
Murphy said these closures have a serious impact on access to health services in the communities the hospitals served. For example, when local hospitals close, patients must travel farther for care, and those needing inpatient treatment are taken by ambulance on trips that can last two hours — leaving ambulances and EMTs unavailable in their own communities, Murphy explained.
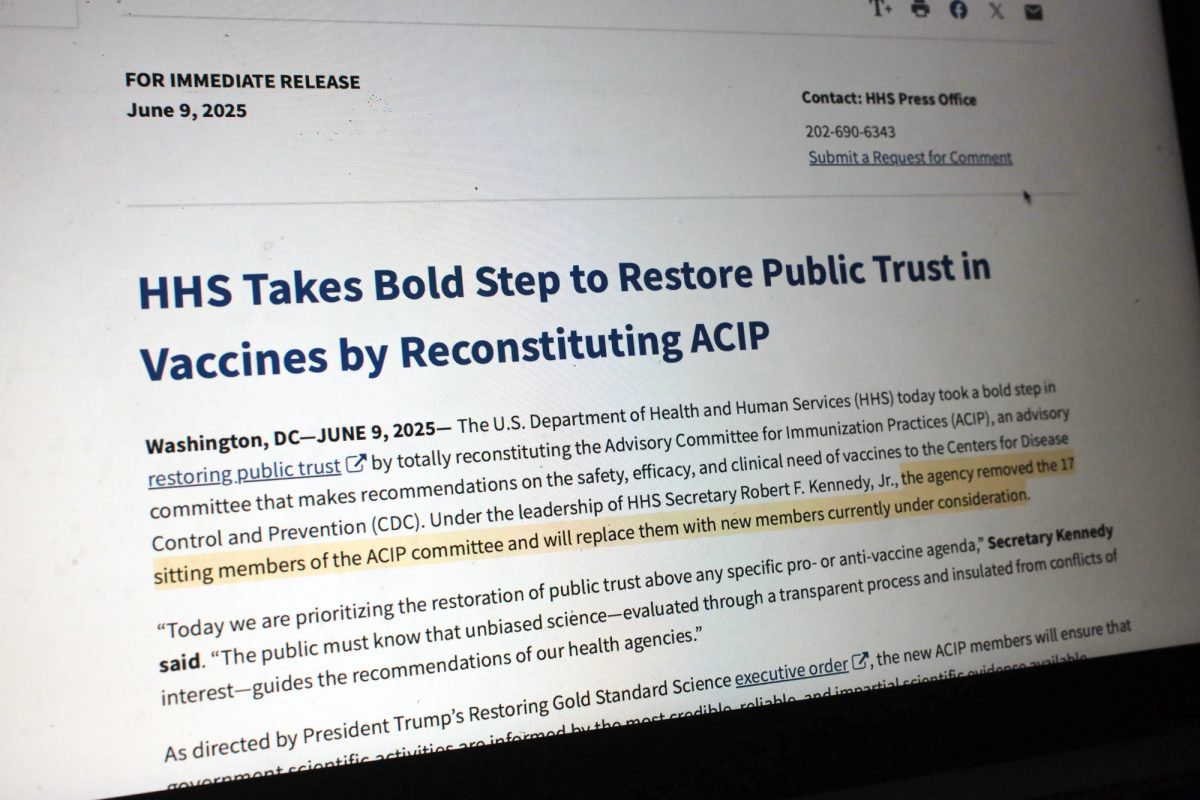
In his testimony, Sager said more steps to be taken to address the inefficiency of health care spending and to prepare for the “political storm bearing down on healthcare,” as a result of this inefficiency.
“Our state needs to prepare,” he said. “When the plane’s motor stops, it’s too late to start sewing parachutes.”